Pulmonary Fibrosis Model
Discover how Melior’s unique phenotypic screening platforms can uncover the untapped value of your candidate therapeutic
Fibrosis is the formation of excess fibrous connective tissue in an organ or tissue in a reparative or reactive process. There are many described types of fibrosis with pulmonary and hepatic fibrosis being the most common.
Pulmonary fibrosis can be caused by chronic inflammatory processes, infections, environmental agents, exposure to ionizing radiation, chronic conditions and certain medications.
Pulmonary fibrosis is characterized by alveolar epithelial cell injury and hyperplasia, inflammatory cell accumulation, fibroblast hyperplasia, deposition of extracellular matrix, and scar formation. The end result of this process is the loss of lung elasticity and loss of alveolar surface area leading to impairment of gas exchange and pulmonary function. The disease is further characterized by the presence of chronic inflammatory infiltrates, myofibroblast hyperplasia, and disordered collagen deposition.
The bleomycin lung fibrosis model is the best characterized, and most widely used pulmonary fibrosis model. Direct delivery of bleomycin to the lung (e.g. intratracheal) causes direct damage to alveolar epithelial cells and induces rapidly developing fibrosis after a single administration. This is followed by the development of neutrophilic and lymphocytic alveolitis within the first week. After the first week, alveolar inflammatory cells are cleared, fibroblast proliferation is initiated, with synthesis of extracellular matrix. The development of fibrosis in this model can be seen biochemically and histologically by day 14 with maximal responses observed between 21- 28 days.
Nintedanib and pirfenidone have been used clinically to treat idiopathic pulmonary fibrosis. Both compounds have been evaluated in our bleomycin lung fibrosis model.
Ready to get started or looking for a custom model?
Contact us today for more information about our bespoke research models and to discuss how we can help you answer your unique research questions.
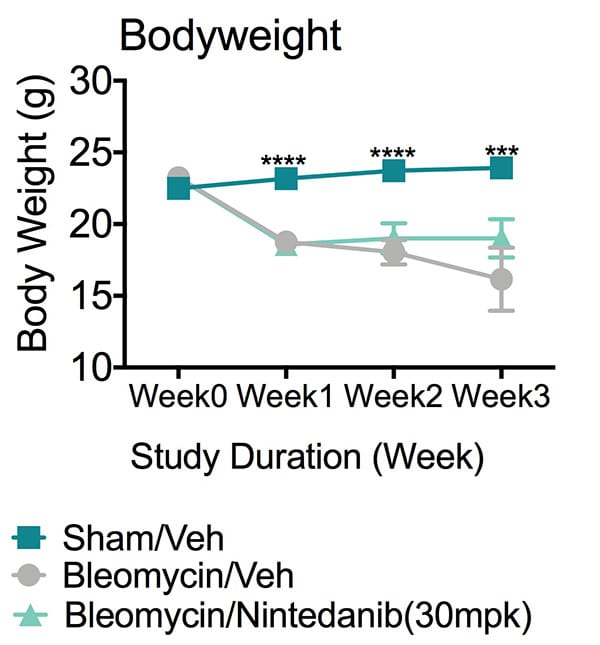
Bodyweight changes. This study was conducted in male C57Bl/6 mice (N=10). Body weights of all animals were recorded on a weekly basis. Compared to animals of Sham/Vehicle group, animals of Bleomycin/vehicle group showed significantly reduced body weights since week1. Data are mean±SEM and analyzed by T-test as applicable (***p<0.01, ****p<0.001, compared to Bleomycin/Vehicle)
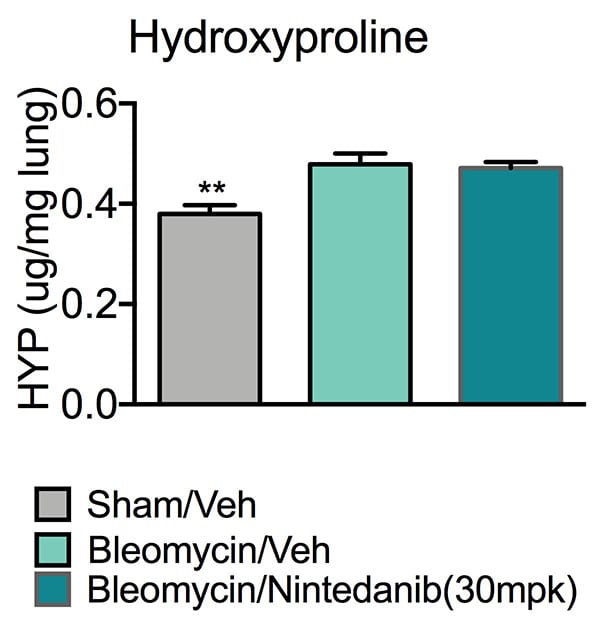
Lung hydroxyproline. On day 21, all animals were euthanized for tissue collection. One side of lung was dissected and used for Hydroxyproline level analysis using Hydroxyproline Colorimetric Assay Kit. Compared to the Sham/Vehicle group, animals of Bleomycin/vehicle group showed significantly increased hydroxyproline level in lung, demonstrating that pulmonary fibrosis has formed. Data are mean ± SEM; **p<0.01 compared to Bleomycin/Vehicle.
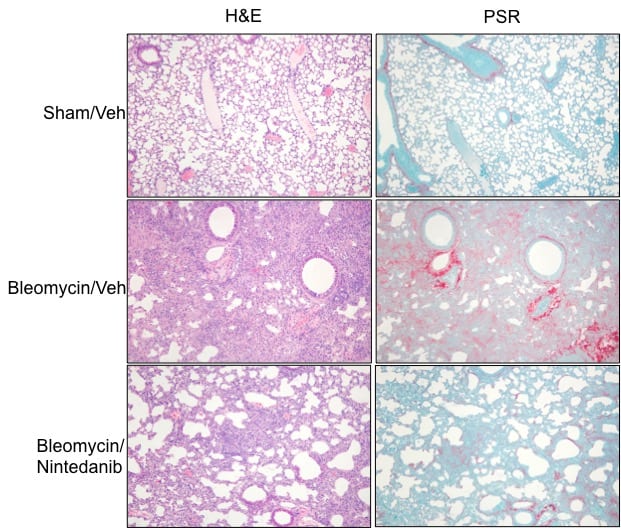
H&E, PSR Staining and Histopathology Score. Hematoxylin and eosin (H&E) and Picrosirius Red (PSR) staining are commonly used histopathology techniques to visualize inflammation and collagen deposit in tissue sections. Pathological alterations were evaluated by an ACVP Board Certified Toxicology Pathologist in blind manner. Interstitial Fibrosis was assessed based on the increase of PSR staining. The subacute interstitial inflammation and Agonal Hemorrhage were evaluated mainly based on the H&E staining. Compared to the lung samples from Sham/Vehicle group, significant increases in both interstitial fibrosis and inflammation were observed in the lung samples of Bleomycin/Vehicle group. Nintedanib treatment significantly improved interstitial fibrosis induced by Bleomycin. Data are mean ± SEM; ****p<0.0001,**p<0.01 compared to Bleomycin/Vehicle.
These data reveal that profound lung fibrosis has been induced by bleomycin and Nintedanib treatment effectively improved the histopathology changes in this bleomycin lung fibrosis model.
Frequently Asked Questions
Pulmonary fibrosis is caused by chronic pulmonary inflammation.
The lung injury following bleomycin comprises an interstitial edema with an influx of inflammatory and immune cells. This leads to the development of pulmonary fibrosis characterized by enhanced production and deposition of collagen and other matrix components.
Absolutely! Our scientist would be more than happy to work with you to determine the best reference compounds to be used for your study.
Synonyms: Bleomycin, lung inflammation, fibrosis