Syngeneic Mouse Models
Custom-made solutions and validated tumor models to accelerate your oncology research
Syngeneic tumor models are an essential part of preclinical immunotherapy research. But with limited data and without an exact-match tumor model your research aspirations can become stunted. Melior creates customized models and experiments that meet your needs. When you partner with Melior, you can confidently and efficiently perform in vivo efficacy evaluations of potential cancer therapies. These include targeted therapy, cytotoxic drugs, antibody therapies, checkpoint inhibitors, and gene therapies. Secure early access to the right model and get data that pushes your oncology R&D forward.
Confidently test your immunotherapeutic agents and combination therapies with syngeneic tumor models
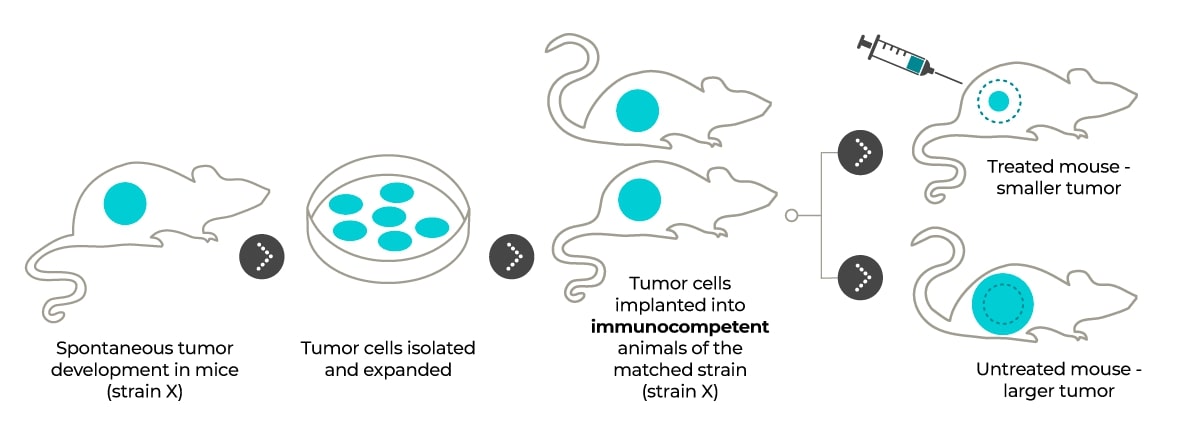
Because syngeneic mouse tumors are immunologically compatible with their host, tumor transplantation does not provoke an immune response apart from potential tumor-specific mediated responses. Instead, tumors grow within an intact immune system. This system provides valuable models for studying therapies that act on the host immune system. With Melior’s syngeneic mouse tumor models, you can develop cancer therapies that work together with the immune system to reduce and reverse tumor growth, as with checkpoint inhibitors.
Advantages of using syngeneic tumor models
- Explore cancer immunotherapies: Get relevant data and better understand the mechanisms of action of new therapeutics targeting immune cell interactions.
- Leverage models with fully competent immunity: Enable studies on the interaction between tumor cells, immune cells, microenvironment, and microbiome.
- Benefit from simple, cost-saving solutions: Generate reliable results with animals inherently less expensive than xenograft models.
Advance your discoveries with our validated syngeneic mouse models
Start your research on the right track by leveraging our expertise and outsourcing your in vivo experiments. Test your immunotherapeutic agents and combination therapies in any of our validated syngeneic tumor models.
Syngeneic Tumor Models
| Disease | Cell line | Strain | Duration | Models | Applications |
|---|---|---|---|---|---|
| Breast carcinoma | EMT6 | BALB | 3 – 4 weeks | Subcutaneous Orthotopic MFP Metastatic | Immunotherapy Chemotherapy |
| Colon Carcinoma | CT26 (CT26.WT) |
BALB | 3 – 4 weeks | Subcutaneous Orthotopic Cecum Metastatic | Immunotherapy Chemotherapy |
| Fibrosarcoma | WEHI164 | BALB/c | 3 – 4 weeks | Subcutaneous | Immunotherapy Chemotherapy |
| Leukemia | L1210 | DBA/2 | 3 – 4 weeks | Intravenous Intraperitoneal Subcutaneous | Immunotherapy Chemotherapy |
| Lewis Lung Carcinoma | LLC (LL/2) |
C57Bl/6 | 3 – 4 weeks | Subcutaneous Intravenous | Chemotherapy |
| Hepatoma | Hepa 1-6 | C57L/J | 5 – 6 weeks | Subcutaneous Orthotopic liver | Immunotherapy Chemotherapy |
| Melanoma | B16F10 | C57Bl/6 | 3 – 4 weeks | Intradermal Subcutaneous Metastatic | Immunotherapy Chemotherapy |
Don’t see what you’re looking for? Contact us for information on other validated models or to discuss a custom solution.
Enhance your study findings with custom services and tools
Seamlessly integrate our additional, bespoke services, such as IVIS imaging, PK studies, IHC, and more, to get the most out of your study.
Syngeneic models: the tool for developing cancer immunotherapies. Syngeneic model tumors are immunologically compatible with their host, and tumor transplantation does not provoke an immune response, apart from potential tumor-specific mediated responses. Benefit from a model with tumors grown in the presence of an intact immune system. To facilitate the study of cancer therapies that work together with the immune system to reduce and reverse tumor growth.
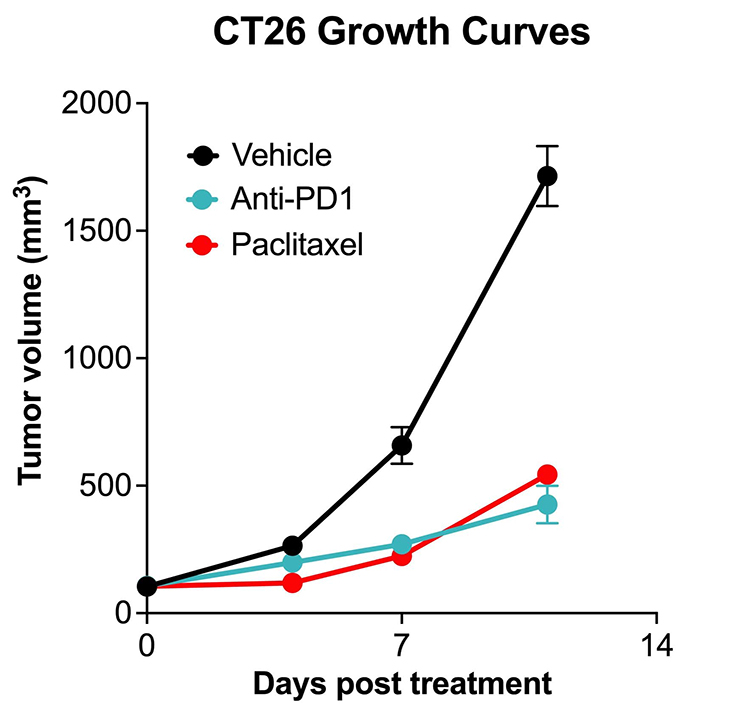
Immune Checkpoint Inhibitor and Chemotherapy Validation in CT26.WT Tumor Model. 1 x106 CT26.WT mouse colon cancer cells were subcutaneously injected into the rear flank of Balb/c mice. Once mean tumor size reached 100-150mm3, mice were randomized into groups and treated with vehicle, anti-PD-1 antibody (12.5 mg/kg IP) once per week, or paclitaxel (20 mg/kg IP) once per week. Tumor growth volume was monitored at baseline and at days 4, 7 and 11, following initiation of treatment, using calipers. Both the anti-PD1 group and paclitaxel group showed significant difference compared with untreated group (both p<0.001; Data area mean ± SEM; n=6 for Vehicle and anti-PD-1; n=4 for paclitaxel).
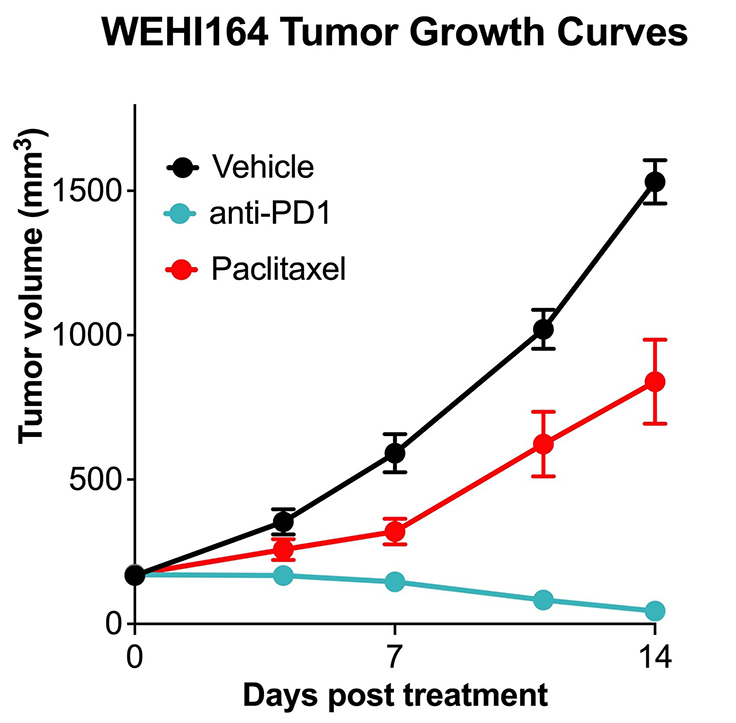
Immune Checkpoint Inhibitor and Chemotherapy Validation in WEHI164 Tumor Model. 1 x106 WEHI164 mouse fibrosarcoma cells were subcutaneously injected into the rear flank of Balb/c mice. Once mean tumor size reached ~150mm3, mice were randomized into groups and treated with vehicle anti-PD-1 antibody (12.5 mg/kg IP) once per week, or paclitaxel (20 mg/kg IP) once per week. Tumor growth volume was monitored at twice per week using calipers. Anti-PD1 significantly inhibited tumor growing. Both the anti-PD1 group and the paclitaxel group showed significant differences compared with the untreated group (both p<0.001; Data area mean ± SEM; n=5 for each group).
Get the data you need with customized experiments and expert advice.
Custom-tailored models for your unique research questions.
Reach your discoveries sooner with industry-leading 4-7 week lead times.
Decades worth of experience across a breadth of research areas.
Publications
Discover the impactful research that our products are facilitating. This selection of publications, authored by researchers like you, underscores our commitment to advancing cancer research and development.
Frequently Asked Questions
Standard subcutaneous models are an efficient choice for measuring tumor response to a new drug. This method involves implanting tumor cells into the flank of a mouse and monitoring growth. Tumors grow efficiently in this model. It allows for analyses such as drug efficacy and endpoint analyses, including survival, flow cytometry, expression analysis, histology, and more.
Orthotopic models, on the other hand, involve seeding tumor cell lines into the corresponding mouse tissue. This strategy assesses tumor development in a relevant tissue environment that mimics the disease process in humans. With orthotopic models, we can monitor and more accurately quantify primary tumor growth, metastatic activity, and response to therapy.
Syngeneic models of lung cancer use tumor cells that are syngeneic to the host; in other words, the tumor cells and the host come from the same species and share a similar genetic background. Typically used in murine (mouse) models, these tumor cells are derived from a mouse strain and are implanted into a mouse of the same strain. This approach allows researchers to study the interaction of lung cancer cells with an intact immune system.
One of the most popular and widely used syngeneic mouse models of lung cancer is the Lewis lung carcinoma (LLC) model. The LLC model utilizes tumor cells from the lungs of a C57BL/6 mouse and is widely used owing to its immunocompetence, thorough characterizations, and consistent tumor growth rates.
Transgenic mice are genetically engineered to carry specific foreign genes, allowing researchers to study gene function, disease development, and genetic disease models. Whereas, syngeneic mouse models are genetically identical within their strain and not genetically modified, making them especially valuable in cancer research and immunology studies. The intact immune system of syngeneic mice makes them ideal for evaluating immunotherapies and understanding the tumor-immune system interactions, offering a controlled environment due to their genetic uniformity.